Urinary incontinence is a widespread yet frequently underreported condition, particularly among women. It affects millions worldwide, impacting not only physical health but also emotional wellbeing and quality of life. Fortunately, with accurate diagnosis and tailored management plans, many individuals can regain control and confidence.
This comprehensive guide explores how to properly assess urinary incontinence, differentiate between its various forms, and implement practical and effective treatment strategies.
What Is Urinary Incontinence?
Urinary incontinence refers to the involuntary leakage of urine, often stemming from dysfunctions in the bladder, urethra, or pelvic floor muscles. It can occur due to numerous causes, and the severity can range from occasional leaks to more significant and persistent loss of bladder control.
Though it affects both genders, women are disproportionately affected, especially after childbirth or menopause. Understanding the type and cause of incontinence is essential for successful management.
Step 1: Comprehensive History Taking and Physical Examination
A thorough clinical history is the foundation for evaluating urinary incontinence. This step extends beyond identifying the incontinence itself – it uncovers overlapping or contributing conditions such as:
- Recurrent urinary tract infections (UTIs)
- Bladder or pelvic pain
- Pelvic organ prolapse
- Neurological conditions
- History of childbirth or pelvic surgery
Questions may include:
- Frequency and timing of leakage
- Fluid intake patterns
- Triggers (e.g., coughing, urgency, exercise)
- Presence of pain or burning during urination
- Obstetric and gynaecological history
- Bowel habits and any straining
A physical examination should assess:
- Pelvic floor muscle tone
- Presence of prolapse
- Abdominal and neurological signs
This information guides the diagnostic process and ensures tailored interventions that address the root cause of symptoms.
Step 2: Assessing Severity and Functional Impact
To measure the severity and impact of urinary incontinence, two tools are commonly used:
1. International Consultation on Incontinence Questionnaire – Urinary Incontinence Short Form (ICIQ-UI SF)
This validated self-report tool provides a structured assessment of:
- Frequency of leakage
- Amount of urine loss
- Impact on daily life
A score of 4 or less is considered mild incontinence, though formal categories for moderate or severe cases are less clearly defined. Still, higher scores suggest the need for more intensive interventions.
2. Bladder Diary or Chart
Patients are asked to track:
- Fluid intake (timing and amount)
- Urine output
- Episodes of urgency or leakage
- Activities associated with leakage
This diary helps distinguish between urge incontinence, stress incontinence, or mixed types and assists clinicians in identifying behavioural or fluid-related patterns contributing to symptoms.
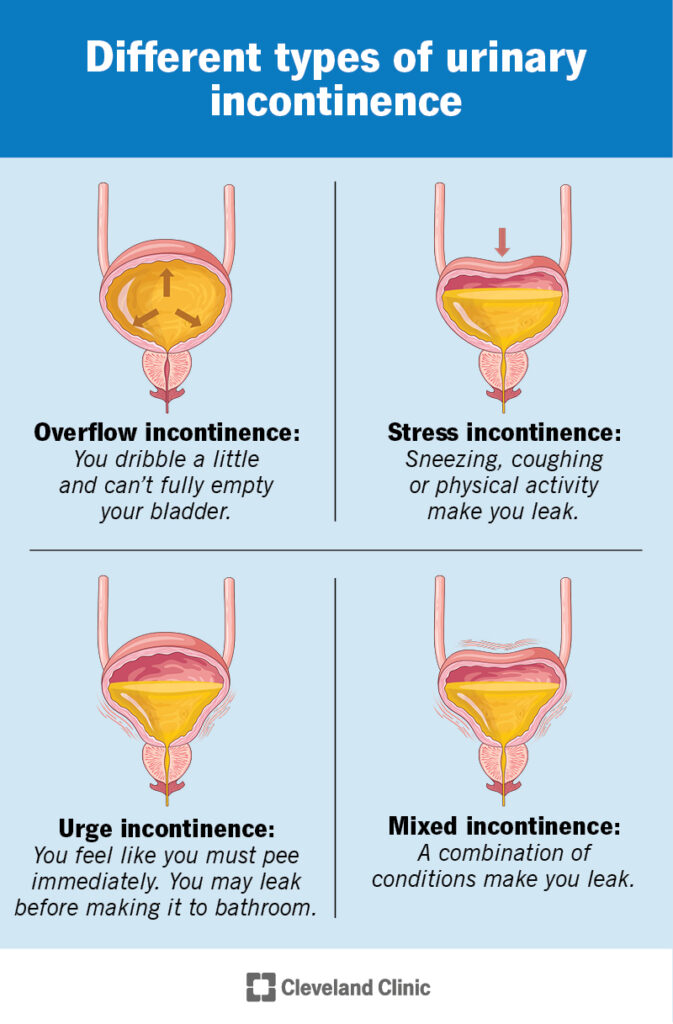
Step 3: Understanding the Types of Urinary Incontinence
1. Urge Incontinence (Overactive Bladder)
Symptoms:
- Sudden, intense urge to urinate
- Leakage before reaching the toilet
- Frequent urination, including at night (nocturia)
Causes:
- Idiopathic or unknown detrusor overactivity
- Obstructive conditions (e.g., bladder stones, tumours)
- Neurological disorders (e.g., multiple sclerosis, Parkinson’s disease)
Management Strategies:
- Bladder Training: Encourage patients to delay urination when the urge strikes. Techniques include:
- Sitting down to reduce urgency
- Contracting pelvic floor muscles
- Mental distraction and controlled breathing
- Medications: Anticholinergic drugs (e.g., oxybutynin, solifenacin) help calm overactive bladder muscles. However, they are not suitable for patients with narrow-angle glaucoma due to risks of increased intraocular pressure.
- Lifestyle Changes: Limit caffeine and alcohol, manage fluid intake, and maintain a healthy weight.
2. Stress Urinary Incontinence
Symptoms:
- Leakage during physical exertion, coughing, laughing, or lifting
Common Risk Factors:
- Vaginal childbirth (especially difficult or prolonged labour)
- Obesity
- Menopause and estrogen deficiency
- Chronic constipation or respiratory conditions (causing frequent straining)
Management Strategies:
- Conservative Interventions:
- Address obesity through exercise and diet
- Manage chronic cough or constipation
- Pelvic Floor Muscle Training (PFMT):
- Supervised or home-based pelvic floor exercises, such as Kegels
- Ideally performed daily for at least 12 weeks
- Improves muscle strength and control, reducing or eliminating leakage
3. Incomplete Bladder Emptying (Voiding Dysfunction)
Symptoms:
- Difficulty starting urination
- Poor or weak urine stream
- Sensation of incomplete emptying
- Post-void dribbling
Common Causes:
- In women: Bladder prolapse, previous pelvic surgery
- In men: Enlarged prostate (benign prostatic hyperplasia)
Management Strategies:
- Double-Voiding Technique:
- Void normally
- Stand up and gently move the pelvis
- Sit back down, lean forward, and relax pelvic muscles
- Promotes further bladder emptying and reduces residual volume
- Advanced Testing:
- If symptoms persist, urodynamic testing can evaluate bladder function in more detail
- Self-Catheterisation:
- In severe cases, intermittent self-catheterisation may be necessary
- Requires careful consideration, education, and hygiene practices
4. Nocturia (Night-time Urination)
Nocturia refers to waking from sleep to urinate, more common with age but often treatable.
Management Techniques:
- Fluid Management:
- Consume most fluids earlier in the day
- Reduce evening fluid intake (limit to small sips)
- Diuretic Use (e.g., Frusemide / LASIX):
- Taking a half-dose diuretic in the morning every other day helps shift fluid from tissues during the day
- Leg Elevation Post-Lunch:
- Encourages fluid movement from lower limbs to the kidneys earlier in the day, reducing night-time urine production
Additional Considerations
When to Refer for Specialist Input
If symptoms do not improve with conservative measures or there are complex factors (e.g., neurological disease, prior pelvic surgery, suspected malignancy), referral to a urologist or urogynecologist may be warranted.
Specialist assessment may involve:
- Urodynamic studies
- Pelvic ultrasound
- Cystoscopy
Restoring Control and Confidence
Urinary incontinence is not just a physical issue—it affects emotional wellbeing, social engagement, and self-esteem. Thankfully, with a structured diagnostic approach and individualised treatment plans, most people can achieve meaningful improvement or complete resolution of symptoms.
Key Takeaways:
- Start with a thorough history and physical examination
- Use tools like the ICIQ-UI SF and bladder diary to guide diagnosis
- Tailor management based on the type of incontinence
- Begin with conservative, non-invasive measures
- Refer to specialists for persistent or complex cases
By empowering patients with knowledge and evidence-based strategies, clinicians can help reduce the stigma of incontinence and significantly enhance quality of life.


